Current Health Issues
The World Health Organization (WHO) recently released a list of 13 urgent health challenges the world will face over the next decade, which highlights a range of issues including climate change and health care equity.
- Climate crisis
- Health care delivery in areas of conflict and crisis
- Health care equity
- Access to treatments
- Infectious disease prevention
- Epidemic preparedness
- Underinvestment in health workers
- Adolescent safety
- Improving public trust of health care workers
- Capitalizing on technological advancements
- The threat of anti-microbial resistance and other medicines
- Health care sanitation.
To address the issue, WHO and its partners are working with low- and middle-income countries to improve hygiene, sanitation, and water conditions at the countries’ health care facilities. WHO also is calling on all countries to ensure all health care facilities have basic hygiene, sanitation, and water services by 2030.

How to build healthy cities and communities post-COVID-19 world
The COVID-19 crisis has illuminated and exacerbated the structural weaknesses of global health systems, especially in urban areas in developed countries as well.
- In the post-COVID world, we must plan and manage cities so as to minimize the risk of disease and ensure equitable access to healthcare.
- The World Economic Forum Healthy Cities and Communities Initiative is tackling health and well-being in Jersey City, Austin, and Mumbai.
The COVID-19 crisis has unveiled the structural weaknesses of not only our economic systems but also, more critically, our health systems. The world is currently confronting the ineptitude of existing health and well-being infrastructure and the consequences of inadequate preventative health mechanisms, particularly for the most vulnerable in society.
Two key variables stand out in this crisis: urbanization and inequality.
Even as urban centers are engines of economic growth, they are challenged by rising physical and mental health concerns among large segments of people.
Unhealthy diets, physical inactivity, environmental conditions, and community and social stress factors are key contributors to this disease burden. As the urban poor have been disproportionately affected by COVID-19, the challenges of urbanization and access to healthy living have catapulted to the forefront of the global agenda.
As we continue to wrestle with the consequences of the crisis and contemplate the post-COVID world, we are left with a critical question to answer:
How will we plan and manage cities so as to minimize the risk of disease and ensure equitable access to healthcare? Our answer to this question will be the foundation of a more healthy, equitable, and just society.
While the call to categorically rethink and reconstruct the nature of our societies is challenging, it presents a unique and necessary opportunity to reshape a future that was already in jeopardy, with looming disasters such as climate change and growing social disintegration.
In a rapidly urbanizing world, it is imperative that cities are not only drivers of economic growth but also centers of health.
The World Economic Forum is responding to this urgent need to re-examine the relationship between cities and population health through its Healthy Cities and Communities Initiative, which launched in September 2019 as a multi-city platform encompassing a full spectrum of developed and emerging economies.
The mission is to empower consumers to achieve long-term health and well-being, with an improved state of holistic health and physical and mental well-being by 2030.
Dimensions ripe for interventions and scaling efforts include:
- Physical well-being (diet, nutrition, sanitation, hygiene, exercise, physical activity, sleep, rest)
- Mental well-being (emotional, social, environmental, spiritual, occupational, financial)

![]()

![]()
Spearheaded by the Platform for Shaping the Future of Consumption, the Forum is working hand-in-hand with cities to improve holistic health and well-being for diverse communities around the world.
The initiative kicked off in the United States in Jersey City, New Jersey – a city with 300,000 residents in 2019 – with the Office of the Mayor of Jersey City and the Department of Health and Human Services.
In nine months, public-private stakeholders have established a secure supply of nutritious food, via locally sourced vertically farmed greens in collaboration with Aerofarms, and provided personalized diagnostics for healthy living with other private sector collaborators.
The initiative has also expedited innovative partnerships on sanitation and hygiene by rolling out Mobile Public Showers.
In July 2020, the collaboration also began in Austin, Texas – a city with over 1 million residents – in partnership with global actors such as IBM and local stakeholder groups such as the Austin Healthcare Council.
The third city is the sprawling metropolis of Mumbai, India, a city with more than 20 million residents. The collaboration began in July 2020 in partnership with the Municipal Corporation of Greater Mumbai and India’s Ministry of Housing and Urban Affairs.
In light of the challenges presented by the coronavirus, sanitation and hygiene have been reemphasized as a key priority, particularly as cities grapple with how to limit contagion in highly dense metropolises such as Mumbai.
Innovative public-private interventions will be taken forward with the Toilet Board Coalition’s India chapter. Just as critical will be other cross-cutting dimensions of physical and mental health such as food and nutrition, physical fitness, mental wellness, rest, and occupational and financial health, with mental health being a critical priority for intervention.
The Healthy Cities and Communities Initiative envisages the creation and improvement of physical, social, and community environments that enable people to lead healthier lives and develop to maximize their potential in a truly inclusive way.
As such, the need for symbiosis between urban planning, economic development, and preventative health has never been greater.
Unquestionably, the process of building truly inclusive health ecosystems within cities will be fraught with challenges and difficulties, yet it is an imperative and a responsibility that we cannot overlook.
What’s the World Economic Forum doing about the future of cities?
Cities represent humanity’s greatest achievements – and greatest challenges. From inequality to air pollution, poorly designed cities are feeling the strain as 68% of humanity is predicted to live in urban areas by 2050.
The World Economic Forum supports a number of projects designed to make cities cleaner, greener, and more inclusive.
These include hosting the Global Future Council on Cities and Urbanization, which gathers bright ideas from around the world to inspire city leaders and running the Future of Urban Development and Services initiative.
The latter focuses on how themes such as the circular economy and the Fourth Industrial Revolution can be harnessed to create better cities. To shed light on the housing crisis, the Forum has produced the report Making Affordable Housing a Reality in Cities.

![]()
Click here for Top 10 Current Health Issues –
Current Health Issues
- Physical Activity and Nutrition
- Overweight and Obesity
- Tobacco
- Substance Abuse
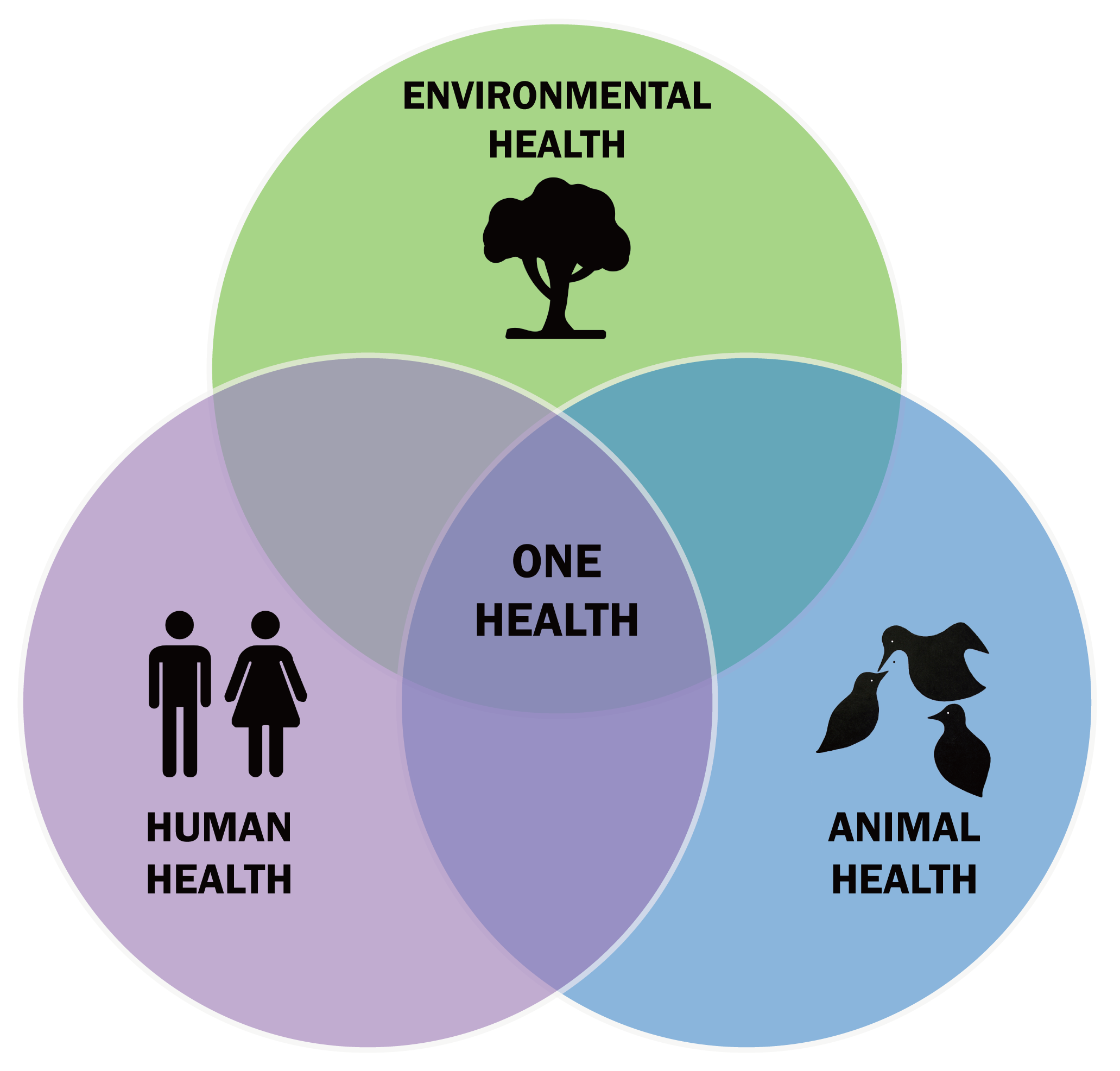
- Mental Health
- Injury and Violence
- Environmental Quality
- Immunization
- Access to Health Care
Physical Activity and Nutrition
Research indicates that staying physically active can help prevent or delay certain diseases, including some cancers, heart disease, and diabetes, and also relieve depression and improve mood. Inactivity often accompanies advancing age, but it doesn’t have to.
Check with your local churches or synagogues, senior centers, and shopping malls for exercise and walking programs. Like exercise, your eating habits are often not good if you live and eat alone. It’s important for successful aging to eat foods rich in nutrients and avoid the empty calories in candy and sweets.
Overweight and Obesity
Being overweight or obese increases your chances of dying from hypertension, type 2 diabetes, coronary heart disease, stroke, gallbladder disease, osteoarthritis, sleep apnea, respiratory problems, dyslipidemia, and endometrial, breast, prostate, and colon cancers.
In-depth guides and practical advice about obesity are available from the National Heart Lung and Blood Institute of the National Institutes of Health.
Tobacco
Tobacco is the single greatest preventable cause of illness and premature death in the U.S. Tobacco use is now called “Tobacco dependence disease.” The Centers for Disease Control and Prevention (CDC) says that smokers who try to quit are more successful when they have the support of their physician.
Substance Abuse
Substance abuse usually means drugs and alcohol. These are two areas we don’t often associate with seniors, but seniors, like young people, may self-medicate using legal and illegal drugs and alcohol, which can lead to serious health consequences.
In addition, seniors may deliberately or unknowingly mix medications and use alcohol. Because of our stereotypes about senior citizens, many medical people fail to ask seniors about possible substance abuse.
Mental Health
Dementia is not part of aging. Dementia can be caused by disease, reactions to medications, vision and hearing problems, infections, nutritional imbalances, diabetes, and renal failure. There are many forms of dementia (including Alzheimer’s Disease) and some can be temporary.
With the accurate diagnosis comes management and help. The most common late-in-life mental health condition is depression. If left untreated, depression in the elderly can lead to suicide. Here’s a surprising fact: The rate of suicide is higher for elderly white men than for any other age group, including adolescents.
Injury and Violence
Among seniors, falls are the leading cause of injuries, hospital admissions for trauma, and deaths due to injury. One in every three seniors (age 65 and older) will fall each year. Strategies to reduce injury include exercises to improve balance and strength and medication review.
Home modifications can help reduce injury. Home security is needed to prevent intrusion. Home-based fire prevention devices should be in place and easy to use. People aged 65 and older are twice as likely to die in a home fire as the general population.
Environmental Quality
Even though pollution affects all of us, government studies have indicated that low-income, racial and ethnic minorities are more likely to live in areas where they face environmental risks. Compared to the general population, a higher proportion of the elderly is living just over the poverty threshold.
Immunization
Influenza and pneumonia and are among the top 10 causes of death for older adults. Emphasis on Influenza vaccination for seniors has helped. Pneumonia remains one of the most serious infections, especially among women and the very old.
Access to Health Care
Seniors frequently don’t monitor their health as seriously as they should. While a shortage of geriatricians has been noted nationwide, URMC has one of the largest groups of geriatricians and geriatric specialists in any medical community in the country.
Your access to health care is as close as URMC, offering a menu of services at several hospital settings, including the VA Hospital in Canandaigua, in senior housing, and in your community.

![]()